Introduction
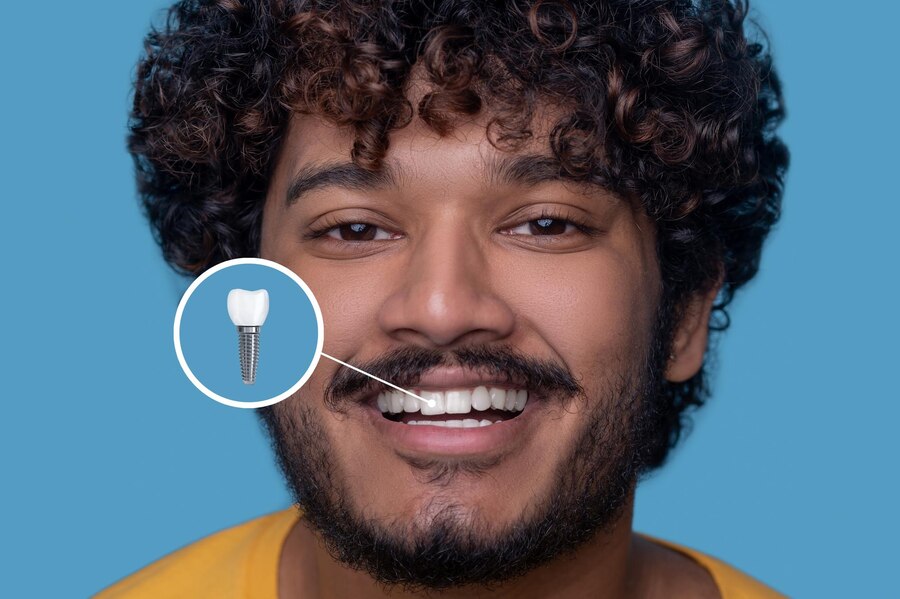
Dental implants are a major investment in your oral health, and following post-procedure guidelines is crucial for a smooth recovery. One common but often misunderstood dietary restriction is avoiding dairy. But why no dairy after dental implant procedures? In this guide, we break down the science and expert advice behind this rule to ensure optimal healing and long-term implant success.
Understanding Dental Implants & the Healing Process
A dental implant involves surgically placing a titanium post into the jawbone, which then integrates with the bone through a process called osseointegration. This critical healing phase determines the implant’s long-term success. Any factor that disrupts healing can lead to complications such as infection, inflammation, or even implant failure.
Key Phases of Dental Implant Healing:
- Immediate Post-Surgery (First 24-48 Hours) – Blood clot formation, swelling, and initial wound healing.
- Early Healing (First Week) – Reduced swelling, soft tissue healing, and prevention of infection.
- Bone Integration (First 3-6 Months) – Osseointegration occurs, solidifying the implant in place.
- Final Recovery & Crown Placement (6+ Months) – The permanent crown is placed, marking the completion of the process.
Any dietary habits that interfere with these healing stages should be avoided—including dairy.
Why No Dairy After Dental Implant?
1. Increased Risk of Infection
Dairy products like milk, cheese, and yogurt contain a high amount of bacteria, which can increase the risk of infection in the open surgical site. Even pasteurized dairy products may still contain bacteria that could trigger an inflammatory response.
2. Disruption of Blood Clot Formation
After implant surgery, a blood clot forms at the site to protect the wound and initiate healing. Dairy consumption has been linked to increased mucus production, which can irritate the surgical site, potentially dislodging the clot and leading to complications such as dry socket or delayed healing.
3. Potential for Inflammation & Delayed Healing
Some individuals are sensitive to dairy and may experience mild inflammation or allergic reactions that slow down the healing process. Inflammation around the implant site can increase discomfort and prolong recovery time.
4. Calcium Interference with Medication
Dairy is rich in calcium, which can interfere with the absorption of certain antibiotics or pain medications prescribed after implant surgery. Poor medication absorption can weaken the body’s ability to fight infections and manage post-operative pain effectively.
5. Risk of Dairy-Induced Nausea
Some people experience nausea or stomach discomfort when consuming dairy, especially after surgery when the body is sensitive. Vomiting after dental implant surgery can increase the risk of complications and stress on the surgical site.
What to Eat Instead? Safe & Nutrient-Rich Alternatives
To ensure proper healing and nourishment, opt for these dairy-free options:
Soft, Nutrient-Dense Foods
- Mashed avocados
- Scrambled eggs
- Smoothies with almond or oat milk
- Soft-cooked vegetables
- Blended soups
- Applesauce
Protein Sources for Faster Recovery
- Lean meats (chicken, turkey, fish)
- Plant-based proteins (tofu, lentils, beans)
- Nut butters (without added sugar)
Calcium-Rich Non-Dairy Alternatives
- Leafy greens (kale, spinach)
- Chia seeds
- Almonds
- Fortified non-dairy milk (almond, soy, oat, coconut)
When Can You Resume Dairy?
Most dentists recommend waiting at least one week before reintroducing dairy into your diet. However, it’s best to consult your dentist before making any dietary changes, especially if you experience prolonged swelling, pain, or signs of infection.
Additional Tips for a Speedy Recovery
- Stay Hydrated: Drink plenty of water to aid healing.
- Avoid Straws: Suction can dislodge the blood clot.
- Maintain Oral Hygiene: Gently rinse with saltwater or prescribed mouthwash.
- Follow Medication Guidelines: Take prescribed antibiotics and pain relievers as directed.
Conclusion
Avoiding dairy after a dental implant isn’t just a precaution—it’s a critical step to prevent infection, inflammation, and delayed healing. By following the right dietary choices and post-surgery care tips, you can ensure a smooth recovery and long-term implant success.